
Abused, Intimidated By A Patient’s Husband, I Was Still Lucky. Other Doctors Or Nurses Might Not Be.
A 2018 ACEP survey of 3,500 respondents, all ER physicians, found that one-third had been punched and spit upon. In 97% of these cases, a patient committed the physical assault, while 28% reported that a patient’s family member or friend was also a perpetrator. About 27% of those assaulted said that the assaults had occurred more than once. As healthcare workers, we constantly deal with the unknown in 24×7 high-stress situations including and beyond medical emergencies, and the unknown can be pretty bad. Here’s a look at the world we inhabit, and a quick idea of some of the internal and external threats that are part and parcel of our daily work life.
By Dr. Nilesh Mehta
A couple of months ago, I was called to see a patient, let’s call her Mrs. T, for an evaluation of anemia. She had a rather protracted and complicated admission to the hospital I’m a consultant at, because of multiple co-morbidities. Due to pandemic restrictions and hospital policy, family members were not allowed to visit inpatient relatives, so we doctors had really no insight into their relatives’ thought processes, and communication between patients and their families was also largely limited to phone calls.
My patient and I, though, had detailed discussions about her diagnosis and testing. She clearly verbalized her understanding and said she had communicated this to her husband. She was advised to see me as an outpatient at my clinic following her discharge. Why am I telling you this story on these pages? Well, what followed was terribly unnerving.
She came to see me at my clinic, along with her husband, and for some reason, he decided to make me the object of his disaffection in no uncertain terms. One minute, I thought I was having a rational conversation, the next minute I was at the receiving end of a big-built, belligerent male subjecting me to a screaming, profanity-riddled tirade, accusing me of treating his wife without consulting him.
The fact that my nursing staff and I had made documented attempts to reach him appeared to hold no water, and his wife’s attempts to calm him down seemed to enrage him further. My goal was to use whatever limited time I had to focus on his wife’s care, but instead, I had to pivot and attempt to deescalate the situation, not just for my sake — he was at least twice my size — but more importantly, for my patient’s. I tried to empathize, and said I understood that the pandemic had made stressful situations even more stressful and that being away from someone you loved was very difficult. He continued to scream abuse at me, before suddenly storming out.
I have to be honest. At that point, my own stress levels were off the charts. Not just because he was much larger than me, but also because I realized I had no idea about him, his background, who he was, or whether he would return with a weapon and attack us. My staff was vulnerable, my patients were vulnerable, and I was vulnerable. Eventually, he did return, and all in all, we were lucky, as his line of attack focused more on bluster, threats, and calling his lawyer, instead of anything physically violent. It was ugly but it could have been far worse.
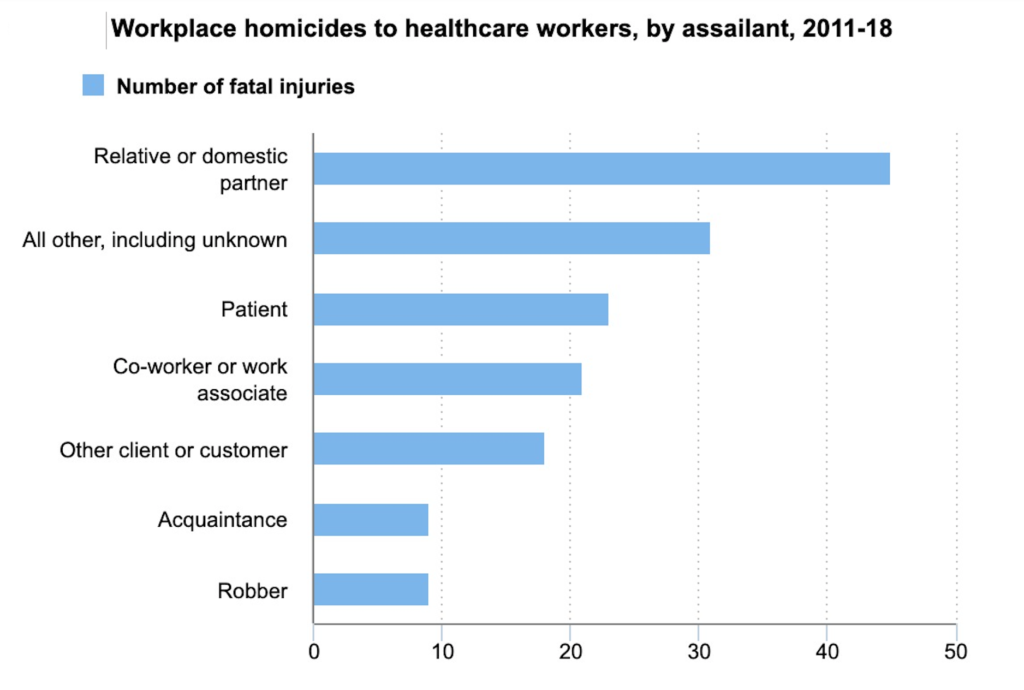
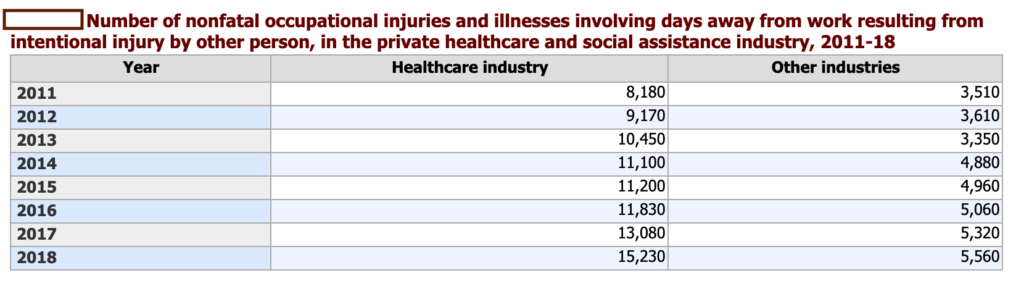
For many other physicians and other healthcare workers across this country, it has been. According to the Bureau of Labor Statistics, from 2002 to 2013, serious workplace violence incidents were four times more common in healthcare settings than in other private industries or offices. Healthcare workers accounted for 73% of all nonfatal workplace injuries and illnesses due to violence in 2018, the most recent year for which this data was made available.
In The Throes Of An Emergency
A Medscape Medical News poll in 2017 of 2,389 people — including nurses, physicians and pharmacists — conducted in the aftermath of the fatal shooting of Dr. Tracy Sin-Yee Tam, a young physician at the Bronx-Lebanon Hospital Center in New York City by an ex-employee, also a physician, found that 88% of respondents said they had personally experienced verbal abuse and 76% said they had experienced intimidation. About two-fifths said they’d been victims of physical assault, and 30% had experienced sexual harassment. Respondents also reported having been stalked. In addition, 55% said they’d witnessed a physical assault in a healthcare setting.
Half of all nurses that responded, 36% of physicians, 18% of pharmacists and 24% of other providers said they had been victims of an assault. The Medscape Medical poll found that nurses in emergency medicine settings had the highest rates of assault — 77% said they’d experienced physical violence — followed by those in psychiatric settings. But 42% of psychiatrists said they’d experienced sexual harassment — compared with 28% of emergency medicine doctors, for instance. Sixty-eight percent of ER physicians said they’d experienced an assault, and an absolutely incredible 99% said they’d been a firsthand witness to violence.
These poll numbers aren’t a surprise. According to the American College of Emergency Physicians (ACEP), nearly seven in 10 ER physicians say emergency department violence is increasing. In a 2018 poll on “Emergency Department Violence,” ACEP reported something rather disturbing: While nearly seven in 10 respondents said that their hospital reported the incident to authorities, only 3% actually pressed charges. But almost 50% believed their hospitals could do more “by adding security, cameras, metal detectors, and increasing visitor screening, especially in the emergency department.”
While visitors, patients or others, are known to be the largest unknown in healthcare settings, employees, current or former, have also been known to have been threats, even lethal ones. Dr. Tam, mentioned above, was shot dead by Dr. Henry Bello, a former Bronx-Lebanon Hospital Center employee, who had quit after sexual harassment allegations. Years earlier, he had reportedly been arrested and charged with sexual abuse after assaulting a woman in Manhattan. Because he pled guilty to a lesser charge, the felony sexual abuse charge was dropped and reportedly did not come up in a background check by the hospital. That June 2017 day, Dr. Bello, armed with an AR-15, killed Dr. Tam and injured six others before killing himself.
The United States has more than 160 million workers. Healthcare and Social Assistance is the largest sector in the United States. According to the US Census Bureau data for 2019, 918,433 businesses in the sector employed in the range of 21 million people. Healthcare is always a high-stress work environment, but in this surreal new world we inhabit, we are on high alert 24×7, dealing with a once-in-a-century pandemic in addition to regular healthcare crises from cancer to substance abuse to gunshot wounds. At both ends of the spectrum, patients and healthcare personnel are experiencing very difficult times.
As I said, I was lucky. My own recent experience in the middle of a busy Chicago day, could have gone very bad very soon. It is often very hard for patients and family members to keep a lid on their emotions, particularly when there is so much frustration all around. As healthcare workers, we need to maintain composure as much as we can in these testing times, but it’s equally important to do everything possible, as hospital systems, to protect ourselves and our patients however we can. We’re human, it helps to know who or what we’re dealing with.
(The writer is a practicing hematologist and oncologist in the Midwest).