In The Wild, Wild West – And East – Of Healthcare Fraud, These Strike Forces Are On A Mission
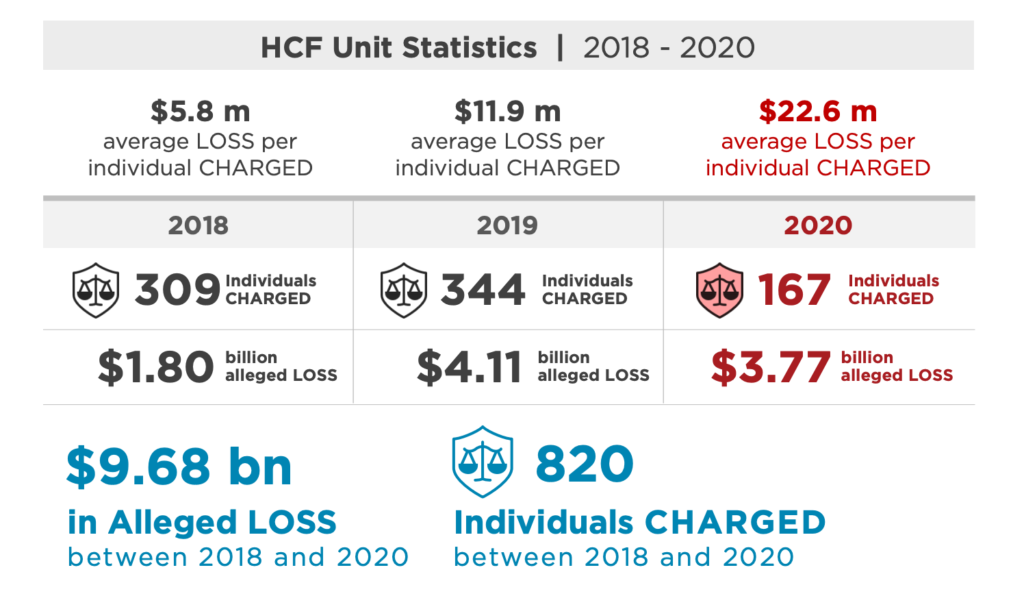
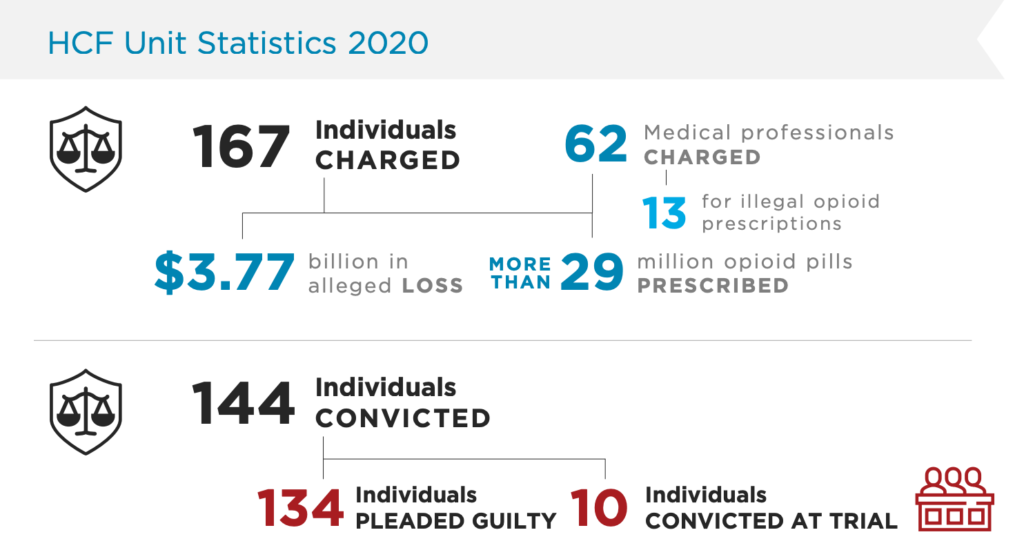
On Feb. 24, the Department of Justice’s Fraud Section released its 2020 “Year In Review.” Sixty-two of the 167 individuals charged last year by the Health Care Fraud Unit were medical professionals, 13 of whom faced charges for illegal opioid prescriptions. Together, they were allegedly responsible for $3.77 billion in fraudulent losses. Today, we look at what healthcare fraud in the United States looks like, and at the teams working to take down illegal health-related operations.
By a Biometrica staffer
On Feb. 25, a federal grand jury in Kentucky returned an indictment against a medical doctor from Dayton, Ohio, and a chiropractor from Union, Kentucky, for their alleged involvement in conspiracies to illegally distribute opioids and commit health care fraud. According to court documents and the Department of Justice (DOJ), Dr. William Lawrence Siefert, 67, and Timothy Ehn, 48, coordinated their reportedly illegal prescribing and health care fraud conspiracies through Northern Kentucky Center for Pain Relief, a pain clinic in Florence, Kentucky. Siefert, was employed by the clinic, while Ehn, the chiropractor, was also the clinic’s owner.
Siefert and Ehn allegedly offered drug-seeking patients who should not have received opioids easy access to these dangerous controlled substances, then billed Medicaid for millions of dollars in medically unnecessary urinalysis testing related to these patients. The indictment alleges that Siefert and Ehn’s alleged illegal opioid prescribing conspiracy was a contributing factor in the opioid overdose deaths of at least six former clinic patients.
The men were each charged with one count of conspiracy to unlawfully distribute controlled substances and one count of conspiracy to commit health care fraud. Siefert was also charged with three counts of health care fraud and 11 counts of illegal distribution of controlled substances, including oxycodone, hydrocodone, and clonazepam, and Ehn was charged with eight counts of health care fraud.
Siefert and Ehn’s allegedly fraudulent practices have not been in isolation. On Feb. 24, the DOJ’s Fraud Section released its 2020 “Year In Review” report. The division has three litigating units, the Foreign Corrupt Practices Act Unit, the Market Integrity and Major Frauds Unit, and the Health Care Fraud (HCF) Unit, but for the purposes of this piece, our focus is on the third division, which is primarily focused on the prosecution of complex health care fraud and cases involving the illegal prescription, distribution, and diversion of opioids.
In 2020, the HCF charged 167 individuals allegedly responsible for $3.77 billion in fraud loss, while 144 were convicted for healthcare related fraud. Sixty-two of those charged were medical professionals, 13 for illegal opioid prescriptions. But just barely two months in and 2021 has already seen a spate of arrests, indictments and sentences handed out against health care providers of different stripes across the country.
On Feb. 18, a Southern California hospice administrator was sentenced to 30 months in prison for his role in a multimillion-dollar hospice fraud scheme. Eighty-year-old Antonio Olivera admitted that from 2011 to 2018, while acting as administrator for Mhiramarc Management LLC, a hospice located in Downey, California, he and others paid illegal kickbacks to patient recruiters for the referral of hospice beneficiaries to Mhiramarc. The co-conspirators caused Mhiramarc to submit approximately $28 million in claims to Medicare, resulting in a $17M+ payout to the company. Three co-conspirators have pled guilty and are awaiting sentencing.
On Feb. 12, two Texans from Katy were charged for their alleged participation in a drug distribution conspiracy perpetrated over the Darknet. Kevin Ombisi, 31, and Eric Russell Jr., 35, who were both arrested on Feb. 11, allegedly used a marketplace on the Darknet and the encrypted messaging service, Wickr, to sell pills made to resemble Adderall. The pills actually contained methamphetamine.
On Feb. 10, a Michigan woman, Amina Abbas, became the first person in the U.S. to face criminal charges for the intentional misuse of funds intended to provide relief to health care providers and maintain the access to medical care during the Covid-19 pandemic. Abbas owned a home healthcare provider company called 1 on 1 Home Health, which she closed in early 2020 after Medicare issued an overpayment demand for $1,619,967.08 because 1 on 1 had allegedly submitted claims for patients who did not qualify for home health services. According to the indictment, 1 on 1, which did not operate during the pandemic, received approximately $37,656.95 designated for the medical treatment and care of COVID-19 patients. Abbas allegedly misappropriated the funds by issuing checks to her family members for personal use.
On Feb. 8, a 73-year-old Ohio physician was sentenced to two years in prison for the unlawful distribution of controlled substances. Dr. Morris Brown, pled guilty on Feb. 21, 2020, after being charged in an April 2019 indictment with four others: Ismail Abuhanieh, 50, of Phoenix, Arizona; Mahmoud Elmiari, 44, of Bellbrook, Ohio; Yohannes Tinsae, 48, of Beavercreek, Ohio; and Mahmoud Rifai, 50, of Detroit, Michigan. All four of Brown’s co-defendants were charged for agreeing to obtain controlled substances by fraud or misrepresentation for Dayton Pharmacy, which leased space in a building owned by Brown. Three of them, Abuhanieh, Elmiari, and Tinsae, have been sentenced pursuant to guilty pleas. Rifai is the subject of an active arrest warrant.
On Feb. 3, Henry McInnis, the 50-year-old CEO of the Merida Group, a Texas-based group of hospice and home health entities, was sentenced to 15 years in prison for falsely telling thousands of patients with long-term incurable diseases they had less than six months to live in order to enroll the patients in hospice programs. He had been convicted in Nov. 2019 of one count each of conspiracy to commit health care fraud, conspiracy to commit money laundering, obstruction of justice, as well as six counts of health care fraud. Rodney Mesquias, the company’s owner, was sentenced to 240 months in prison in December 2020. From 2009 to 2018, McInnis, Mesquias and others submitted more than $150 million in fraudulent claims for hospice and other health care services. McInnis had no medical training and worked previously as an electrician.
On Jan. 15, a Hattiesburg, Mississippi, businessman was sentenced to 18 years in prison and ordered to pay $287,659,569 in restitution for his role in a multimillion-dollar scheme to defraud TRICARE, by distributing compounded medications that were not medically necessary. TRICARE is the health care benefit program serving U.S. military, veterans, their families and private health care benefit programs. Wade Ashley Walters, 54, a co-owner of numerous compounding pharmacies and pharmaceutical distributors, had pled guilty to one count of conspiracy to commit health care fraud, and one count of conspiracy to commit money laundering. Walters was also ordered to forfeit the $56,565,963 he personally derived from the fraud scheme.
On Jan. 11, Ivan Andre Scott, the 34-year-old owner of an Orlando-area call center, was convicted for a kickback scheme that resulted in the payment of approximately $2.8 million in false and fraudulent claims to Medicare. He was convicted of one count of conspiracy to commit health care fraud, three counts of health care fraud, one count of conspiracy to defraud the United States and pay and receive health care kickbacks, and three counts of receiving kickbacks. According to the DOJ, Scott targeted Medicare beneficiaries with telemarketing phone calls falsely stating Medicare covered expensive cancer screening genetic testing. After beneficiaries agreed to take the test, the evidence showed Scott paid bribes and kickbacks to telemedicine companies to obtain doctor’s orders authorizing the tests.
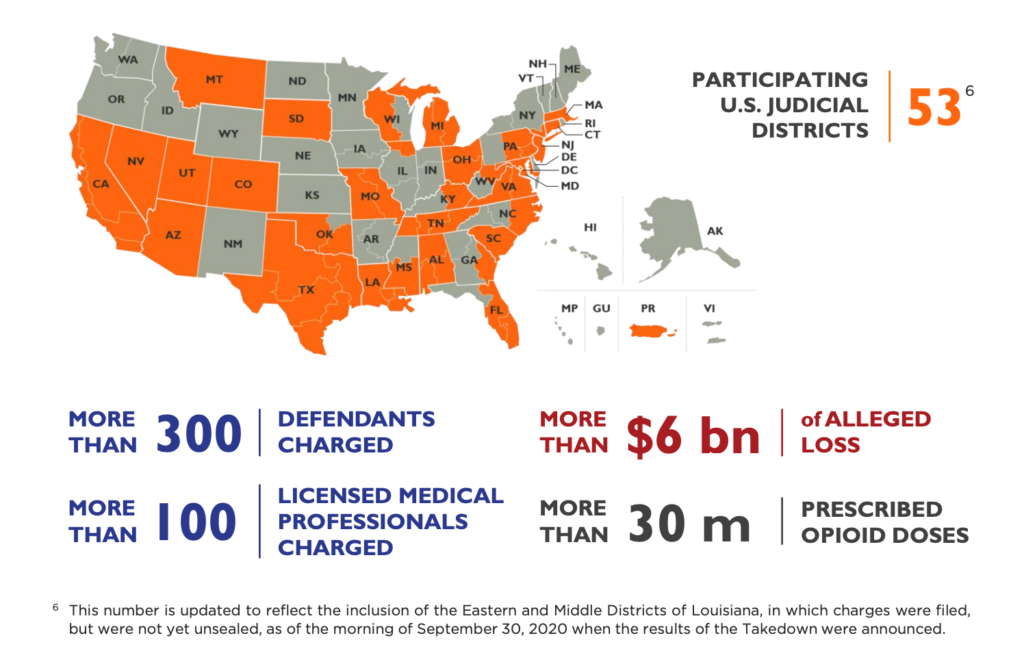
When most people think of crime and criminal conspiracies, they rarely think of healthcare providers or healthcare fraud. But here’s an interesting stat: Since the time of its creation in October 2018, the Appalachian Regional Prescription Opioid (ARPO) Strike Force, which operates in 10 districts, has charged 91 defendants, including 68 licensed medical professionals, and its casework has targeted the alleged illegal distribution of more than 65 million controlled substance pills involving more than 350,000 prescriptions. These actions have resulted in more than 41 convictions till Dec. 31, 2020.
Additionally, since its own inception in March 2007, the Health Care Fraud Strike Force, which maintains 15 strike forces operating in 24 districts across the U.S., has charged more than 4,200 defendants who have collectively billed the Medicare program for approximately $19 billion.
What Exactly Are These Strike Forces?
According to the DOJ, the Health Care Fraud Strike Force (Strike Force) model consists of interagency teams made up of investigators and prosecutors that focus on the worst offenders engaged in fraudulent activities, including, chiefly, health care fraud, wire fraud, mail fraud, bank fraud, money laundering offenses, violations of the Anti-Kickback Statute, false statements offenses, Title 42 offenses, Title 26 offenses, and Title 21 offenses, in the highest intensity regions.
These investigators use advanced data analysis techniques to identify aberrant billing levels in health care fraud “hot spots” – cities with high levels of billing fraud, in addition to traditional investigative techniques, to target suspicious billing patterns and look for emerging schemes and fraudulent practices that migrate from one community to another.
The Strike Forces bring together the FBI, the Department of Health and Human Services Office of Inspector General (HHS-OIG), the Centers for Medicare & Medicaid Services (CMS) Center for Program Integrity (CPI), and other agencies (e.g., DEA, IRS-CI, USSS, FDIC-OIG, DOD-OIG, USPIS, DOL-OIG, DCIS), and the HCF Unit’s internal Data Analytics Team, along with the prosecutorial resources of U.S. Attorney’s Offices and state and local law enforcement partners.
The ARPO Strike Force was set up under the aegis of the DOJ’s Criminal Division and is a collaboration between the DOJ, FBI, HHS-OIG, DEA, and state and local law enforcement to combat health care fraud and the opioid epidemic in parts of the country that have been hardest hit by addiction. Its primary focus is on the prosecution of medical professionals and others involved in the illegal prescription, diversion, and distribution of opioids.
Then we have the DOJ’s latest baby, the National Rapid Response Strike Force (NRRSF), whose mission is to quickly respond to multi-jurisdictional health care fraud cases and priorities. NRRSF prosecutors, based in Washington, D.C. and in some existing Strike Force locations, also coordinate with U.S. Attorneys’ Offices and federal and state law enforcement partners to prosecute these significant multi-jurisdictional and corporate fraud matters.
Also, in September 2020, the Criminal Division announced the “Sober Homes Initiative,” the first coordinated enforcement action in DOJ history focused on fraud schemes in the substance abuse treatment industry. Led by the National Rapid Response, Los Angeles, and Miami Strike Forces, with the participation of the U.S. Attorneys’ Offices for the Central District of California and the Southern District of Florida, the initiative focuses on schemes intended to exploit patients suffering from addiction. To date, according to the Fraud Unit’s Year in Review report, the Sober Homes Initiative has resulted in 13 individuals charged for roles in various schemes to defraud health care programs of more than $934 million.