Nursing Home Covid-19 Cases Rose Sharply Last Week As Staff Vaccination Rates Still Lag
By a Biometrica staffer
The number of nursing home patients and staff infected with the Covid-19 virus rose sharply last week, at a time when the nation is reeling under the menace of the highly contagious delta variant and as total cases in the U.S. have climbed to a six-month high with over 100,000 infections. States that have lower vaccination rates have been ravaged the most, overall, with the recent surge affecting unvaccinated people more severely than others.
On Thursday, Aug. 5, White House chief medical advisor Dr. Anthony Fauci warned that a more severe Covid variant could emerge, while also estimating that there are roughly 93 million people nationwide who are eligible for the vaccine but haven’t received it yet. Healthcare systems are under immense strain and are running out of space in Florida, Georgia, and Louisiana, which account for almost 40% of all hospitalizations in the country.
Louisiana and Georgia have some of the lowest vaccination rates in the nation. In Florida, hospitals are using everything from conference rooms and auditoriums to cafes to set up more beds. The Biden administration, meanwhile, is said to be developing a plan that requires nearly all foreign visitors to the United States to be fully vaccinated against Covid-19 as part of a plant to eventually lift the travel restrictions that currently bar much of the world from entering the country.
Now, against this backdrop, the lag between vaccination rates among nursing home staff and nursing home residents is back in the limelight. On July 22, the Associated Press reported that the Centers for Disease Control and Prevention (CDC) was investigating facilities in the Grand Junction, Colorado, area that was hit hard by the recent surge in cases. The federal investigation, which suggested a link between lagging vaccination rates among nursing home staff and a national spike in infections, found that many nursing home workers were not inoculated.
In that article, the AP said that about 59% of nursing home staff have been vaccinated nationally, about the same as the overall percentage of fully vaccinated adults. However, that rate was significantly lower than the roughly 80% of residents vaccinated. The CDC investigation raised concerns that successes in protecting vulnerable elders with vaccines could be in peril as the more aggressive delta variant spreads across the country, combined with a lag in the vaccination rates among staff.
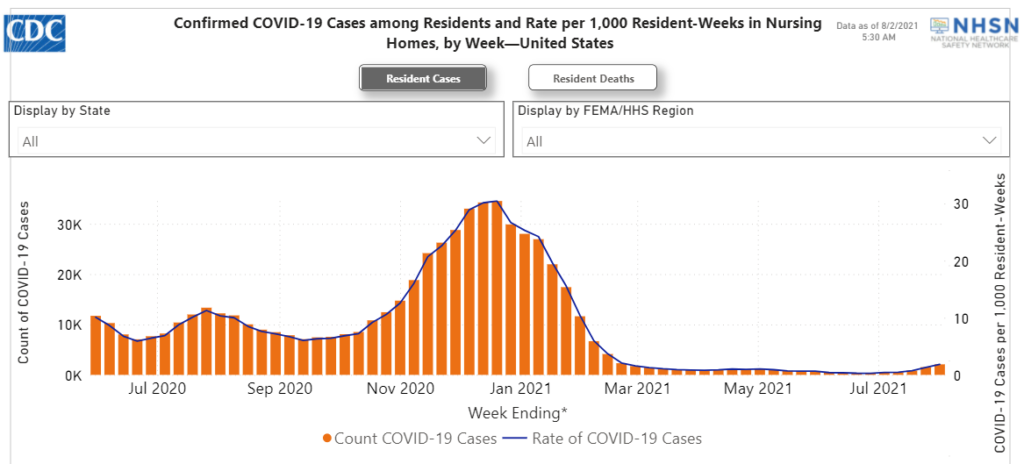
CDC data for the most recent week, i.e., between July 25 and Aug. 1, shows that Covid-19 cases among nursing home residents rose 38% to 2,041 from 1,478, NBC reported. Florida’s long-term care facilities account for more than a quarter of the cases, with 564, up from 348 the previous week. The number of nursing home residents who died of Covid-19 nationwide rose to 281 last week from 163. Cases among nursing home staff jumped 31% to 3,252 from 2,467 in the last week.
Whenever there’s been a rise in cases in the community, it’s been known to infiltrate nursing homes, Dr. Morgan Katz, an assistant professor of medicine at the Johns Hopkins School of Medicine is quoted as saying by NBC News. Much of the reason behind this, though, is that only 60% of the nursing home staff is vaccinated, which allows the virus a potential entry into the facility, Katz added.
Some experts have been urging the government to close the gap by requiring nursing home staffers get shots. “Vaccinating workers in nursing homes is a national emergency because the delta variant is a threat even to those already vaccinated,” Dr. Joshua Sharfstein, vice dean for public health practice at Johns Hopkins Bloomberg School of Public Health, was quoted as saying in the AP report from July 22. But some nursing home operators have expressed concerns that a mandate could backfire and prompt staffers who are skeptical of getting the vaccine to simply quit, at a time when the load on the healthcare system is already extremely high.
Still, a couple of states have begun to issue such mandates. Massachusetts Gov. Charlie Baker’s administration announced on Wednesday, Aug. 4 that all unvaccinated employees and contractors at skilled nursing facilities in the state will be required to get their first vaccine shot by Sept. 1 and be fully vaccinated by Oct. 10. California went one step further on Thursday when it issued a mandate that requires all healthcare workers to be inoculated, allowing only for religious or rare medical exemptions. Employees of hospitals, nursing homes, doctors’ offices, clinics, and other medical facilities have until Sept. 30 to get at least one dose of the vaccination, under the new order.
And it’s not just state governments that are mandating vaccinations for nursing staff.
Genesis Healthcare, which has 70,000 employees at nearly 400 nursing homes and senior communities, announced this week that its employees must get the shot to keep their jobs. Nursing home residents, even those who have been inoculated, are more vulnerable than many other demographics because many are elderly and frail, with weak immune systems. The mandate by Genesis Healthcare suggests that private facilities may be willing to risk an exodus, despite already dangerously understaffed homes, to quickly vaccinate those still resisting shots and fend off the surging delta variant, the AP reported.